



There was a time when anyone could access data on deaths in India. Not anymore. At least, the information seems to be missing from censusindia.gov.in.
The information is crucial as the country battles the coronavirus outbreak. Certified deaths would have helped us know the number of people who died of COVID-19, the respiratory disease caused by the coronavirus. Without this perspective, the conclusions we draw could be erroneous.
As the certificate would have the cause of death, it would step up pressure on the government to improve health services, which, in turn, would mean a healthier India.
Today, the website continues to exist but has information about deaths only till 2014. So, there is an annual report on Medical Certification of Cause of Death (MCCD) for each year till 2014. There is no annual report thereafter.
A possible reason could be an issue raised by the then Deputy Registrar General, RK Gautam. In his August 28, 2014 letter to all state registrars, Gautam bemoaned the fact that deaths were not being medically certified. He said “. . . the present coverage to medically certified deaths to the total registered deaths is 20.2% and only 14.3% against the total estimated deaths”.
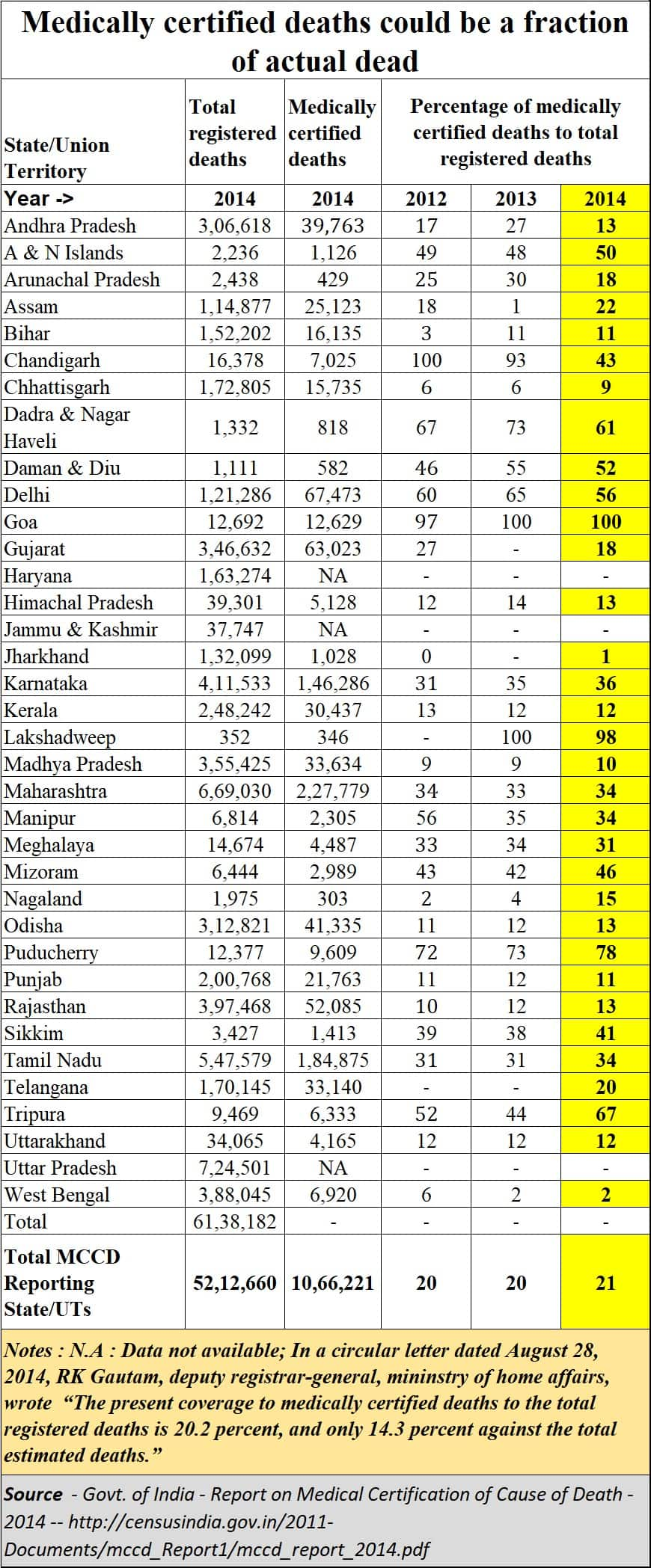
This was just before the latest MCCD report—2014--came into the public domain. It is from this report that the table alongside has been excerpted.
The report shows that almost 80% of the deaths registered are without medical certification.
This means that the COVID-19 death certification would belong to the 21% of certified deaths if the same percentages are relevant even today.
Given the paucity of doctors, it is reasonable to believe that the percentage of medically certified deaths has not increased.
More worrying is that many deaths are not even registered. That would mean that people die without anyone knowing about it. This is borne out by researchers Mudit Kapoor and Shamika Ravi, who were with the Indian Statistical Institute and Brookings Institute, respectively, when they wrote this article, when they say “in large and less developed states such as Uttar Pradesh and Bihar, 62 percent and 74 percent of the births, respectively, were registered, while only 38 percent and 43 percent of the deaths, respectively, were registered. Overall, in India, 85 percent of births and 74 percent of deaths were registered.”
In other words, 26 percent of the deaths are not even registered. And only 21% of the registered deaths are medically certified–going by the 2014 report.
What this also points to is that India does not have enough doctors to ensure that all deaths are certified. This is unfortunate when we see the number of patients milling around government hospitals. India offers an opportunity for setting up a few hundred more medical colleges since patients are there to be diagnosed and treated.
After they have been taught the theory, the only way students become good doctors is by dealing with lots of patients.
Instead, successive governments–have over the past five decades–opted to promote private medical colleges, many of which appear to be more interested in making money than imparting quality education.
The fact that many Indian students go overseas for medical education is another pointer to the latent demand–and inadequate medical seats–in India.
One of the big problems India faces in the coronavirus outbreak is the shortage of medical staff. This needs to be addressed urgently.
To make it possible, India needs to spend a lot more on health services and augment the numbers of both hospitals and medical staff.
Yet, just two years ago, the government appeared keener on upgrading those trained in ayurvedic, homeopathic and unani schools of medicines to be allopaths if they appeared for a bridge course than increase medical seats.
It is dangerous to interfere with the sanctity of any professional certification programme. Fortunately, doctors have challenged this move and the matter is now with the courts.
There is another worrying issue that needs to be addressed. The disappearance of such data from the public domain means that India’s policymakers have to depend on the information provided by bureaucrats, who can be wily.
The best way policymakers can arrive at the right solution is by crowd-sourcing opinion. That is possible only when people have access to data. By not sharing the data, policymakers end up making themselves, and the country, more vulnerable. It was to check this vulnerability and to empower people that the Right to Information Act was introduced.
The Kerala High Court recently observed that the registration of birth and death is mandatory under the Registration of Birth and Death Act, 1969, and all citizens are bound to follow it. Under the Act, death could be recorded at any time, the court said, calling for a penalty if the law was not followed, media reports have said.
The government, it said, needed accurate data for welfare schemes. That is the reason the data missing from the website is a gaping hole that should be plugged at the earliest.
(The author is a consulting editor with Moneycontrol.)Discover the latest Business News, Sensex, and Nifty updates. Obtain Personal Finance insights, tax queries, and expert opinions on Moneycontrol or download the Moneycontrol App to stay updated!
Find the best of Al News in one place, specially curated for you every weekend.
Stay on top of the latest tech trends and biggest startup news.