
Hypertension is frequently referred to as the “silent killer” because it doesn't have obvious symptoms, and often goes undiagnosed. If left unchecked, it can inflict health problems including but not limited to vision loss, kidney failure, stroke and heart attack.
Today, as per the World Health Organization (WHO), hypertension is the number one cause of deaths globally - accounting for 7.5 million deaths per annum. Hypertension is a significant risk factor for cardiovascular diseases, accounting for approximately 30 percent of deaths globally. Thus it is a pervasive health issue impacting millions of human beings.
Understanding the importance of maintaining normal blood pressure for general well-being and longevity is essential. Today, on World Hypertension Day, here's a look at how to recognize the problem early on and find ways to prevent this deadly disease.
Why are Indians more susceptible to hypertension?
Due to several factors such as the Indian diet (high in foods with added sodium), genetic predisposition, and socioeconomic and lifestyle factors, India is progressing towards being hypertensive. As per a study in the Journal of Hypertension, the prevalence of hypertension in India is among the highest, with almost 30 percent of the Indian population suffering from it. Some studies have also suggested South Asians, including the Indian population, are more susceptible to hypertension. This rise is also evident with the recent spurt in deaths due to heart attacks in the younger population. And above all, the lack of awareness and access to good medical care for this disease is a genuine concern.
What is normal blood pressure?
The force of the blood flowing through and exerting pressure on the wall of the blood vessels is known as blood pressure. The unit in which it is measured is a millimetres rise of mercury (mmHg), expressed in systolic and diastolic blood pressure. Systolic pressure is when the heart contracts forcefully and beats, creating more blood flow pressure in the blood vessels. Diastolic pressure is the pressure in the blood vessels when the heart rests between the beats. The suitable range of this pressure to be maintained in the human body is less than 120 systolic pressure and 80 diastolic pressure, or 120/80 mm/Hg, as per the American Heart Association (AHA).
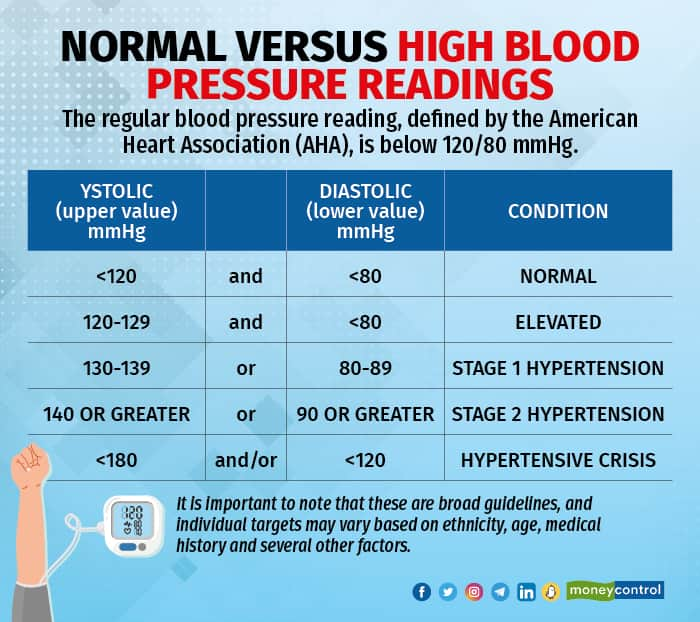 Source: AHA
Source: AHA
A growing body of evidence points towards the importance of sustaining stable blood pressure, which decreases the risks of heart attack, stroke and kidney disease.
How is blood pressure measured, and who needs an ambulatory BP machine?
Traditionally, blood pressure is measured using a sphygmomanometer with the blood pressure cuff wrapped around the upper arm and inflated. As the cuff inflates, it compresses the brachial artery, transiently inhibiting blood flow.
As the pressure in the cuff slowly releases, the pressure on the artery reduces. Through the stethoscope, the healthcare professional listens to the blood pulsing through the artery as it begins to flow again. This pressure in the artery is the systolic pressure – the initial or the top number in the blood pressure reading. The second or bottom number is known as diastolic pressure, which is heard as the pressure continues to drop until no more sounds are heard.
The ideal management of hypertension has long been debated, with health experts and researchers perpetually seeking the best approach to minimize the risk of cardiovascular events such as heart attack and strokes due to hypertension. However, regular monitoring of one’s blood pressure levels is where there is consensus in the medical fraternity concerning its management. The traditional in-the-doctor's-office blood pressure measurements offer meaningful insights into one’s risk, but they may not capture the entire picture of one’s blood pressure because of the ‘white coat effect’ – which means one’s blood pressure readings tend to be higher in a medical setting.
Continuous monitoring of blood pressure, which goes beyond eradicating the white coat effect, can track the blood pressure variability (BPV), which is the blood pressure fluctuation level across the day. It has become a hot topic in medical research and is now regarded as a vital indicator of cardiovascular health.
Various factors influencing BPV are lifestyle, underlying medical condition and age. One common misconception I want to remove through this article is that many believe hypertension is a natural part of ageing and is normalized.
While blood pressure may gradually increase with age, succumbing to it can be avoided with certain lifestyle factors that I’ll highlight in this article. Thus, we should aim to prevent it and not accept that it is normal to become hypertensive with age. The idea may be natural when we follow a sedentary lifestyle with poor sleep and diet. But living with high blood pressure is certainly not worth the pleasure of such a poor lifestyle.
Why is it important to keep track of blood pressure variability, or BPV?
Studies have shown that high BPV is strongly linked with a higher risk of kidney damage, cognitive decline and adverse cardiovascular events. Research published in the American Heart Association's Hypertension journal revealed that people with greater BPV had a 25 percent higher risk of all-cause mortality and a 15 percent higher risk of stroke.
An ambulatory blood pressure monitoring (ABPM) can help you accurately assess BPV, which involves wearing a portable, small device for 24 hours. It takes blood pressure readings at regular intervals throughout the day and night. It gives a comprehensive overview of blood pressure fluctuations, enabling your physician to customize more effective treatment. Thus, ABPM is the gold standard for evaluating BPV and crafting treatment plans.
Managing BPV is of prime importance in reducing the risk of life-threatening complications. Lifestyle interventions such as regular exercise, daily 10,000 steps, a wholesome minimally processed food intake, reduced intake of added processed salt and active stress management can prevent, mitigate and even reverse hypertension in some cases. Furthermore, regular blood pressure monitoring is critical for early detection and prevention.
 A wrist monitor for measuring blood pressure (Photo by Shvets Production via Pexels)
A wrist monitor for measuring blood pressure (Photo by Shvets Production via Pexels)
Hypertension science: how we know what we know
The landmark Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) conducted between 1994 and 2002 involving over 42,000 volunteers has been vital in guiding physicians to prescribe the most effective treatment for hypertension. ALLHAT documented that thiazide diuretics, specifically chlorthalidone, which works by eliminating excess sodium and water from the body, is the most affordable and effective treatment option for treating hypertension as it reduces the risk of heart failure significantly compared with other lines of treatments such as angiotensin-converting enzyme (ACE) inhibitors and calcium channel blockers (CCBs). So for most patients, thiazide diuretics remain the recommended first line of treatment. However, the study also highlighted that healthcare providers should consider a patient’s unique circumstances and health history when prescribing antihypertensive medication and customized treatment plans’ significance.
Another trial conducted between 2010 and 2015, the Systolic Blood Pressure Intervention Trial (SPRINT), offers meaningful insights into the aggressive treatment of hypertension and the correlated risks. SPRINT was a multicentre, randomized, controlled trial designed to assess the benefits of aggressive hypertension treatment. It involved volunteers aged 50 years or older with systolic blood pressure (SBP) between 130-180 mmHg and an enhanced risk of adverse cardiovascular events. The intensive treatment group received medication to keep a target of <120 mmHg SBP, and the standard treatment group participants were treated to maintain an SBP of <140 mmHg. The primary or hard outcomes examined were severe adverse cardiovascular events such as heart failure, heart attack, stroke and cardiovascular mortality. The secondary outcomes assessed were all-cause mortality, cognitive function, kidney disease and quality of life.
However, the SPRINT trial was prematurely stopped after a median follow-up of 3.26 years due to immense benefits observed in favour of intensive treatment, with a 25 percent reduction in the primary composite outcome and a 27 percent reduction in all-cause mortality compared to the standard treatment group. These outcomes point to the fact that aggressive treatment for hypertension could enormously lower the risk of adverse cardiovascular events and mortality rates in patients with hypertension. Due to these insights, in 2017, the American College of Cardiology and American Heart Association (ACC/AHA) updated their guidelines for effectively managing blood pressure by incorporating the SPRINT trial findings. As per the new guidelines, the diagnosis of hypertension is an SBP of 130 mmHg or more.
Finally, it is better to be proactive and take steps to keep blood pressure at normal levels for better overall health and longevity. Regular monitoring is the first step to managing healthy levels of blood pressure. Additionally, we shouldn’t normalize high blood pressure as a problem of ageing, but do what it takes to prevent it.
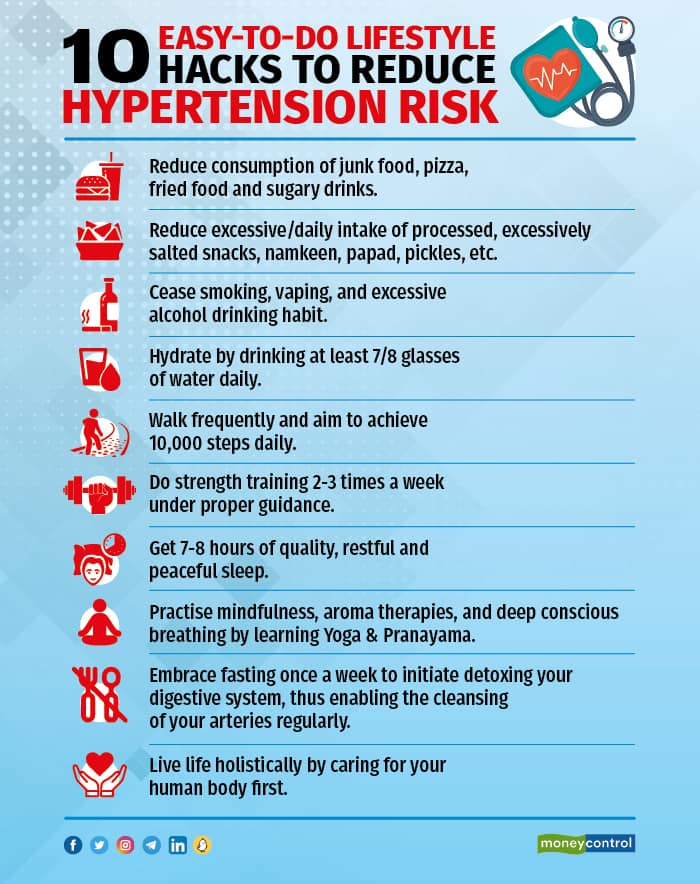
If necessary, consult a medical professional and seek medical intervention. Monitoring and preventing hypertension will help us decrease the risk of this life-threatening complication and help us live and enjoy a higher quality of life, even as we age gracefully.
Discover the latest Business News, Sensex, and Nifty updates. Obtain Personal Finance insights, tax queries, and expert opinions on Moneycontrol or download the Moneycontrol App to stay updated!