



India, our majestic and bustling nation, is home to over a billion people, each with a story to tell. Now, imagine if almost a third of these individuals were bearing the burden of heavy backpacks. That is the symbolic weight many Indians carry due to weight-related issues.
These issues are far from trivial; they have unceremoniously crowned India the “diabetes capital of the world,” with over 100 million residents grappling with the condition. Heart diseases have claimed the top spot among causes of death. The culprit? Our compromised metabolic health is a dark cloud that looms menacingly over the nation.
Envision metabolic diseases, also known as metabolic syndrome, as an evil parade, with the “four horsemen” at the forefront:
- Diabetes
- Cardiovascular disease
- Cancer
- Neurodegenerative disease
Signs of metabolic syndrome (MetSyn)
To truly wrap our heads around metabolic disease, we must recognize that being metabolically unhealthy extends beyond the realms of excessive weight and high blood sugar.
Let’s venture back to the 1980s, when Gerald Reaven, a visionary endocrinologist, first identified “Syndrome X.” This condition included five symptoms, which are:
- Truncal obesity – Excessive fat accumulation around the trunk area
- Elevated triglycerides levels
- Depressed HDL cholesterol
- High blood pressure
- Elevated glucose levels
These symptoms were found to be strongly correlated with the development of diabetes, cardiovascular disease, cancer, and neurodegenerative diseases.
Fast forward to the present, and Syndrome X has metamorphosed into what we now know as metabolic syndrome (MetSyn). The criteria for diagnosing MetSyn, as agreed upon by the American Heart Association and the National Heart, Lung, and Blood Institute, include:
- Truncal obesity is defined as having a waist circumference of 40 inches or more for men and 35 inches or more for women.
- Elevated triglyceride levels are defined as having 150 mg/dL or higher or taking medication for elevated triglyceride levels. Triglyceride levels less than 100 mg/dL are preferred.
- Low HDL cholesterol levels (the particles that remove cholesterol from our body and are considered good) are defined as less than 40 mg/dL in men or less than 50 mg/dL in women or taking medication for low HDL cholesterol levels.
- Blood pressure of 130/85 mmHg or higher or taking medication for high blood pressure. A blood pressure lesser than 120/80 is preferred.
- Elevated fasting glucose is defined as having levels of 100 mg/dL or higher or taking medication for elevated glucose levels. The preferred level is 80 mg/dL.
When one has three or more of these risk factors, it is enough to be diagnosed with metabolic syndrome. However, it is essential to note that having even one of these risk factors is worse than having none. Each additional risk factor compounds the risk of developing chronic diseases. Think of metabolic syndrome as a series of dominoes. When they tumble, a cascade of chronic diseases can ensue.
Metabolic syndrome and increased risk for heart disease, cancer and neurodegenerative diseases like dementia
The risks associated with poor metabolic health are profound. Let’s delve into some startling statistics underscoring MetSyn’s far-reaching impact.
Cardiovascular disease
A substantial body of research, including a comprehensive systematic review and meta-analysis published in the Journal of the American College of Cardiology, which examined 87 studies covering over 951,000 patients, unequivocally demonstrates the adverse effects of MetSyn on cardiovascular health. Here are some staggering statistics:
- The risk of cardiovascular disease in people with metabolic syndrome surges by 135%.
- The risk of cardiovascular mortality (death) escalates by 140%.
- The risk of all-cause mortality rises by 58%.
- Heart attack risk amplifies by 99%.
- Stroke risk swells by 127%.
Cancer
Turning our attention to cancer, a study published in the European Journal of Cancer uncovered the following:
- MetSyn is linked with a 56% age-adjusted increase in the risk of cancer mortality.
- Several specific types of cancer are substantially more likely to occur in individuals with MetSyn:
- Endometrial (uterus) cancer – sevenfold increase in likelihood.
- Esophageal cancer – nearly fivefold increase.
- Gastric cancer – approximately twofold increase.
- Liver and kidney cancers – roughly twofold increase.
The National Cancer Institute highlights that metabolic syndrome and being overweight or obese are significant drivers of cancer risk. While smoking remains the top environmental trigger of cancer, obesity sits in the second position.
When we take a closer look, it becomes evident that metabolic syndrome, which often overlaps with obesity, is a significant factor in cancer risk.
Neurodegenerative diseases
Now, let’s explore the relationship between metabolic health and neurodegenerative diseases.
Parkinson’s disease: The largest meta-analysis on this topic, published in the journal PLoS Medicine, indicates a 24 percent increased risk of Parkinson’s disease in individuals with metabolic syndrome compared to those without. Furthermore, the risk is graded, with three risk factors resulting in a 31 percent increased risk and all five risk factors leading to a 66 percent increased risk.
Alzheimer’s disease: Research published in the journal Nutrition, Metabolism and Cardiovascular Diseases points to a 10 percent increased risk for Alzheimer’s among those with MetSyn. While this may seem relatively low, it is essential to note that Alzheimer’s disease paradoxically appears to have a protective role, contributing to a 16 percent reduction in obesity. This observation is likely due to reverse causality, where Alzheimer’s disease can lead to weight loss.
Other forms of dementia: Considering all forms of dementia, including vascular dementia, Lewy body dementia, and frontotemporal dementia, vascular dementia exhibits a 37 percent increase in risk.
Thus, the correlation between metabolic syndrome and the heightened risk of diabetes, cardiovascular diseases, cancer, and neurodegenerative diseases is a stark reminder of the crucial importance of maintaining optimal metabolic health. The evidence is clear – once you have metabolic syndrome, you are at an elevated risk of “everything.”
Limitations of body mass index (BMI) and body weight as indicators of metabolic health
Standing on a weighing scale or measuring your BMI is like looking at a summary of a complex book: the numbers give you a glimpse, but they might not tell the whole story of your metabolic health.
In the quest to assess our metabolic health, we often rely on the seemingly straightforward metrics of body weight and body mass index (BMI). These metrics are like the cover of a book; they give us an overview, but they can be deceiving.
Let’s take a closer look at the relationship between obesity and metabolic health. In the US, a study by the National Institute of Diabetes and Digestive and Kidney Diseases in 2021 found that among 108 million obese adults (defined as having a BMI over 30), 62 percent or 67 million individuals also had metabolic syndrome.
 Uncoupling Obesity from Metabolic Health
Uncoupling Obesity from Metabolic Health
However, a significant one-third of the 100 million people in the USA diagnosed with metabolic syndrome were not obese. This data is like a plot twist in a novel, revealing that obesity and metabolic syndrome do not always go hand in hand.
Now, if we turn the page and evaluate the effectiveness of BMI and weight as indicators of metabolic syndrome risk at an individual level, we see their limitations. They fail to consider crucial factors like body composition and insulin sensitivity. Like a muscular athlete with a high BMI due to muscle mass, is at a lower risk of metabolic syndrome.
 Poster issued by the US National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health, Public Health Service, US Dept. of Health and Human Services. (via Wikimedia Commons)
Poster issued by the US National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health, Public Health Service, US Dept. of Health and Human Services. (via Wikimedia Commons)
How to assess metabolic health
So, how do we unlock the actual narrative of our metabolic health? Instead of relying solely on body weight, we should use a variety of tests and metrics to paint a more accurate picture of our health:
- Uric acid
- Homocysteine
- Triglycerides/HDL-C ratio
- Fasting Glucose and Insulin
- Hemoglobin A1c
- Liver function tests
- Oral Glucose Tolerance Test (OGTT)
- Continuous Glucose Monitoring (CGM)
- DEXA Imaging Scan
- Liver Ultrasound
These tests are like chapters in a book, each providing crucial information that contributes to a comprehensive understanding of our health. By looking at these metrics, we can have a clearer picture of our metabolic health, just as we would have a fuller understanding of a book by reading each chapter.
Let’s start by understanding the ideal ranges for these metrics:
Uric Acid: Males should aim for 2.5-7.0 mg/dL, ideally below 5 mg/dL.
Females should strive for 1.5-6.0 mg/dL, again, ideally below 5 mg/dL.
Homocysteine: Target 5-15 μmol/L, with an optimal range below 9 μmol/L.
Triglycerides/HDL-C Ratio: The recommended guideline is below 5:1, but ideally, we want to aim for a ratio where triglycerides are less than HDL cholesterol, so <1:1.
Fasting Glucose: Ideally, this should be below 99 mg/dL. However, since various factors can influence this metric, relying on continuous glucose monitoring (CGM) can provide a more accurate picture.
Fasting Insulin: Aim for below 20 μU/mL, with an ideal range of below 8 μU/ml or possibly even closer to 6.
Hemoglobin A1c: Strive for below 5.7 percent, as levels at or above this indicate prediabetes and above 6.5 percent is confirmed diabetes. Again, CGM is a reliable alternative.
Liver Enzymes: Alanine Transaminase (ALT) should range from 7-36 units per litre of serum, with an ideal range below 23. Aspartate Transaminase (AST) should be between 8-33 units per litre of serum, also ideally below 23.
 Visceral adipose tissue, or the fat stored in the abdominal cavity, acts like an active hormone-secreting (endocrine) organ, producing hormones and cytokines known as adipokines, which can contribute to inflammation and various metabolic diseases. (Photo by v2osk via Unsplash)
Visceral adipose tissue, or the fat stored in the abdominal cavity, acts like an active hormone-secreting (endocrine) organ, producing hormones and cytokines known as adipokines, which can contribute to inflammation and various metabolic diseases. (Photo by v2osk via Unsplash)
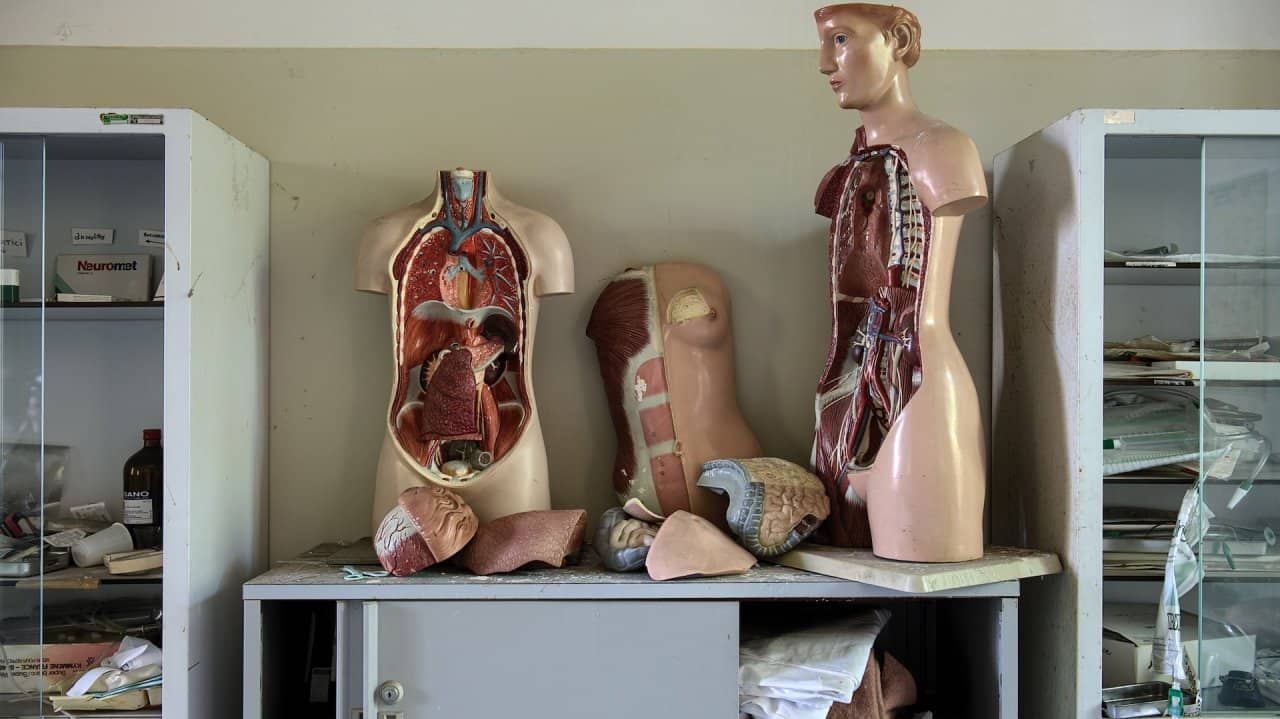
Visceral Adipose Tissue (VAT): Fat around the vital organs
Next, let’s delve into the fat surrounding our vital organs, such as the liver, muscle and pancreas, known as VAT, or visceral adipose tissue, and its impact on our health. VAT is the fat stored in the abdominal cavity, and it’s pretty different from the subcutaneous fat stored just under our skin. VAT acts like an active hormone-secreting (endocrine) organ, producing hormones and cytokines known as adipokines, which can contribute to inflammation and various metabolic diseases.
A helpful way to visualize fat storage is the “bucket analogy.” Imagine a bucket that represents the capacity of our subcutaneous fat, the safe storage depot for excess energy. People have different-sized buckets, and the size correlates with how much fat can be stored without adverse health outcomes. If your bucket is small, you might be thin but metabolically unhealthy, as any additional fat spills into VAT. Conversely, if you have a large bucket, you can store more fat without it spilling over into VAT, potentially making you obese but still metabolically healthy.
Here are three specific ways VAT can contribute to health issues:
Muscle Cells: Fat accumulation can reduce the muscle’s capacity to respond to insulin, leading to insulin resistance.
Intrahepatic Fat: This fat can increase triglyceride-rich, cholesterol-poor, very low-density lipoprotein (VLDL) particles in circulation, ultimately increasing the risk of developing blockage in arteries supplying blood to the heart, increasing the risk of heart attack and cardiac arrest.
Peripancreatic Fat: This fat can be toxic to the beta cells in the pancreas that produce insulin, impairing insulin production and contributing to type 2 diabetes.
It’s essential to understand that you don’t need a lot of VAT to cause health issues; even a tiny amount can have significant adverse impacts. On a DEXA scan, a healthy goal for VAT levels is under the 10th percentile.
Metabolic Health Assessments: The Oral Glucose Tolerance Test (OGTT) and Continuous Glucose Monitors (CGMs)
The Oral Glucose Tolerance Test (OGTT) provides insights into the body’s response to the carbs we consume that ultimately gets broken down into glucose and potential warning signs for type 2 diabetes (T2D). Here’s how it works:
Here's how the test is done: You'll need to fast for 12 hours before the test. Once you're at the lab, a technician will take a baseline blood sample to assess initial glucose levels. Then, you'll be asked to drink a glucose solution containing 75g of pure glucose, and remain seated and inactive for the duration of the test. Three more blood samples will be taken at intervals of 30 minutes over the next two hours to measure glucose and insulin levels.
The OGTT is particularly valuable as it can detect type 2 diabetes (T2D) even in individuals with a haemoglobin A1c level below the diagnostic threshold of 6.5 percent. As per a 2017 study published in the reputed journal Diabetologia, the critical marker is when blood glucose levels reach 200 mg/dL at the 120-minute mark, clearly indicating T2D.
Continuous Glucose Monitors (CGMs) are an excellent tool to overview one’s metabolic health comprehensively. CGMs offer a range of data, including average blood glucose levels, frequency of blood glucose peaks, the time taken to return to baseline levels after peaks, and the correlation between blood glucose peaks and various lifestyle factors such as meals, stress, or exercise. CGMs are particularly useful as they directly calculate average blood glucose levels, avoiding potential inaccuracies that can arise with haemoglobin A1c measurements.
It’s essential to remember that haemoglobin A1c results can be affected by factors such as the turnover rate of red blood cells and abnormal red blood cell size. Therefore, if the OGTT reveals any anomalies, it is recommended to use a CGM for at least 30 days to get a comprehensive overview of your metabolic health.
Liver function and Non-alcoholic fatty liver disease (NAFLD)
Liver function is a pivotal aspect of metabolic health, with Non-alcoholic fatty liver disease (NAFLD) affecting 33 percent of Indians. Identifying this condition is crucial and relies on various diagnostic tools and tests.
Key Indicators of NAFLD
Slight elevations in transaminases, including ALT (alanine aminotransferase) and AST (aspartate aminotransferase).
Liver ultrasound and fibrosis score provide a more holistic view of the liver’s health, detecting the presence of fat, fibrosis, and scarring.
The early stages of NAFLD are entirely reversible. However, if not addressed promptly, it can progress to Non-alcoholic steatohepatitis (NASH), which, while still reversible, can eventually lead to cirrhosis if fibrosis sets in. In fact, NAFLD is now a leading cause of liver transplants in India.
Notably, liver fat fibrosis, a condition traditionally linked to excessive alcohol consumption, is increasingly observed in non-alcoholic cirrhosis cases, often resulting from diets high in refined sugars and fats.
Diagnostic Tools for Liver Fat Accumulation:
- CT scans or MRIs.
- FibroScan is an ultrasound that utilizes various biomarkers.
- Interestingly, elevated transaminase levels in the 30s range have become normalized due to their population-wide prevalence. However, optimal levels should generally be in the 20s.
Lifestyle Interventions: The Power of Non-Pharmacological Strategies
In the realm of metabolic health, lifestyle interventions play a critical role. Timely testing, managing stress, ensuring adequate sleep, regular exercise, and a balanced diet are vital components of a holistic approach to health. These non-pharmacological methods can significantly improve overall well-being.
When it comes to cardiovascular diseases, lifestyle factors are just as important as medical interventions like lipid-modulating medications. Adopting a healthy lifestyle can markedly reduce the risk of atherosclerosis or arterial blockages.
Similarly, with cancer, while certain factors may be beyond our control, early and aggressive screening can facilitate early detection and improve outcomes. Here, too, lifestyle factors play a role in prevention.
 Exercise helps to prevent fat accumulation around the muscles, which in turn affects insulin uptake. (Image via Canva)
Exercise helps to prevent fat accumulation around the muscles, which in turn affects insulin uptake. (Image via Canva)
Exercise as Medicine
Exercise is a vital component of metabolic health, affecting various aspects of our lives, including sleep, nutrition, and ageing. Structurally, exercise improves the strength of joints, muscles, and bones, thereby supporting our mobility as we age. Regarding metabolism, exercise enhances our body’s ability to process glucose, thereby improving insulin sensitivity and potentially preventing type 2 diabetes (T2D).
- Lack of physical exercise can lead to fat accumulation around muscles, disrupting insulin signalling.
- Active individuals develop a mechanism where muscle contractions help glucose enter the muscle without insulin, which is beneficial for those with type 1 diabetes (T1D).
- Both strength training and cardio training have their unique advantages in managing glucose levels.
- Regular physical activity is essential for promoting metabolic health and preventing metabolic disorders.
- Aim to engage in at least 150 minutes of cardiovascular exercise weekly and two weekly strength training sessions.
Nutrition as Medicine
Maintaining energy balance, where caloric intake is in line with expenditure, is crucial for metabolic health. This balance is essential even for non-obese individuals who may be at risk of metabolic diseases.
Approximately 20 percent of non-obese individuals are metabolically unhealthy, exhibiting one or more risk factors for metabolic syndrome. This statistic places them at an equal or even higher risk of metabolic diseases compared to obese individuals with metabolic syndrome. This situation raises the question: how does energy balance matter for non-obese individuals who are naturally in balance due to their weight?
To answer this, let’s consider the “bucket analogy.” The “bucket” represents the body’s subcutaneous fat storage capacity. Those with a small “bucket” have limited fat storage capacity and quickly store excess fat around their organs. Conversely, those with a large “bucket” are likelier to store more fat but are less likely to harm their organs. This point underscores the importance of energy balance in maintaining metabolic health.
A study published in the New England Journal of Medicine 2004 explored the uncoupling of body fat and metabolic health. In this study, subjects with T2D and metabolically healthy subjects underwent liposuction, significantly reducing body weight, BMI, and waist circumference. However, no changes in blood pressure, blood glucose, insulin levels, cholesterol, or triglycerides were observed 12 weeks post-surgery. This lack of progress was because the procedure only removed subcutaneous fat, leaving visceral fat (VAT) intact. This assertion highlights the importance of safely storing fat in subcutaneous spots in the body.
Improving energy balance positively affects the liver, pancreas, and viscera health, with dietary strategies and energy intake playing a crucial role. While exercise can tip the energy balance towards increased output, it doesn’t have a meaningful long-term effect. Instead, consider exercise a tool for improving insulin sensitivity and rely on dietary intake to achieve energy balance.
 Improving energy balance positively affects the liver, pancreas, and viscera health, with dietary strategies and energy intake playing a crucial role. (Photo via Pexels)
Improving energy balance positively affects the liver, pancreas, and viscera health, with dietary strategies and energy intake playing a crucial role. (Photo via Pexels)
Strategies for Energy Balance:
Caloric Restriction: Monitor and consume preplanned food portions.
Dietary Restriction: Eliminate or reduce consumption of energy-dense, nutrient-poor foods, such as processed food added with sugar, white flour and fats.
Time Restriction or Intermittent Fasting: Cycle between periods of eating and fasting to reduce overall caloric intake. Standard intermittent fasting methods include the 16/8 method (fasting for 16 hours and eating during an 8-hour window) and the 5:2 diet (eating normally for five days and significantly reducing calorie intake on two non-consecutive days).
Irrespective of your approach to ensure prolonged satiety, add at least 25 grams of protein per meal or consume 1.6 grams per kilogram of body weight daily.
Sleep as Medicine:
Adequate sleep is often overlooked but is integral to optimal metabolic health. Sleep deficiency of less than 6 hours per night can lead to insulin resistance and an increased risk of diabetes. Additionally, 8 hours per night of sufficient sleep helps manage cortisol levels, which can otherwise negatively impact metabolic health.
Thus, the choices we make in our daily lives have a profound impact on our metabolic health. The ball is in our court; the power is in our hands. Let’s make the right choices and lead a healthy and fulfilling life.
Discover the latest Business News, Sensex, and Nifty updates. Obtain Personal Finance insights, tax queries, and expert opinions on Moneycontrol or download the Moneycontrol App to stay updated!