



India is in a 21-day lockdown to stem the spread of the rampaging coronavirus that has sickened at least 724 people and killed 17. While announcing the decision to keep 1.3 billion people locked indoors, Prime Minister Narendra Modi said the virus could spread at a lightning speed and overwhelm even the best healthcare systems in the world, as he went on to cite the examples of Italy, France and other countries.
India’s healthcare system is poor and would not be able to handle an outbreak, experts have warned. In his address to the nation, Modi also announced a Rs 15,000-crore package to strengthen healthcare. The money should have come much earlier but for that India would have had to take the human development index a lot more seriously. But we didn’t and it shows.
Track this blog for latest updates on coronavirus outbreakIndia spent barely 1.28% of its GDP on health services in 2017-18, figures released by the government in October 2019 show.
In a digital age, it is worrying that the latest data on health, education or agriculture, all of the key sectors of the economy, is not available.
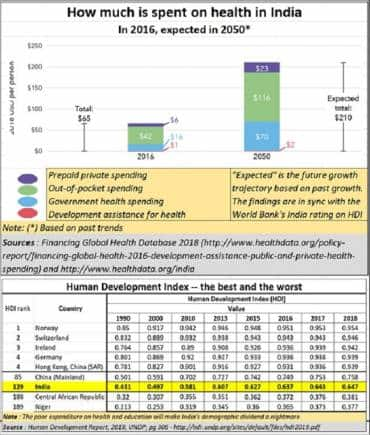
According to the National Health Profile (NHP), 2019, health expenditure in 2015 was just 3.4% of the general expenditure. Our neighbouring countries spent around 8.5% on healthcare. Perhaps that is why India lags almost all developed and developing countries on the index.
The same NHP report says India recorded 4,19,96,260 cases and 3,740 deaths from acute respiratory infection in 2018. In the same year, 7,59,004 cases and 4,105 pneumonia deaths were recorded.
These numbers are significant because the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) causes respiratory distress and attacks the lungs.
With government facilities lacking, people are forced to turn to the private sector and it is expensive. Several studies have shown that debt incurred to pay medical bills is one of the biggest reasons for poverty in India.
The government has set up primary health centres (PHCs) across the country but they are ill-equipped to provide secondary or tertiary care. They are of little help in times like these. They can’t test for coronavirus.
As testing is vital to check the spread of the virus, the ICMR had said if private clinics were allowed, they should offer free tests and get the money reimbursed by the government. But, it has been decided that private clinics will charge patients Rs 4,500 per test, one of the 12 ‘approved’ private pathology companies said in an investor teleconference on March 24.
People who can’t afford the test will go without it or be forced to go to a poorly managed government centre. Not just testing, isolation wards, which are needed to keep infections in check, in government hospitals have common toilets – a major source of infection -- and unsanitary conditions.
Had its health services been good, India could have opted for measures other than a lockdown. It could have adopted the Singapore model. The city-state has not shut schools or offices and its people do not wear masks. But they are not letting the guard down. There is constant monitoring and testing, and the confirmed cases are isolated immediately and treated.
Or, it could have done what Japan is doing. Japan has reported 49 deaths, so far. The country has adopted a “don’t ask, don’t tell” strategy based on minimal testing and buttressed by information massage. It treats the ones identified. But like Singapore, it too has ensured national calm and continued economic activity.
Both countries have depended on information technology and a medical system geared to tackle emergencies and offer the finest healthcare services.
India could have done the same had its healthcare system been dependable, without crippling the economy that would only add to hardship.
Govt has to let goIt is important that the government takes a step back and a new system is put in place to improve healthcare in India.
One good option is through the insurance regulator. Why should the insurance regulator get involved?
First, because it deals with medical insurance. Second, because as of now, it does not reimburse people for their pathology expenses. This is unfortunate because testing allows people to know the health risks they face. This will allow insurance companies to recommend preventive measures to reduce the risk for both the individual and the insurance sector.
For instance, had the insurance regulator been overseeing the medicare sector, it could have reached a deal with developers: Mumbai and its neighbourhood have around 3 lakh unsold flats, with entire apartment blocks lying vacant. It will take builders five years to sell this stock. These apartments could have been rented at a nominal rate to hospital chains for the period and converted into isolation wards, each room with a toilet. The costs would be manageable if the entire insurance sector, with government subsidy for the crisis, backed it.
Insurance companies can give their customers a 60% rebate on pathology tests. It is a win-win for all. It will lead to a decline in out-of-pocket expenditure and people will have an incentive to take medical policies. Insurance companies will benefit because of high registrants and the pathology firms will gain because insurance companies can drive volumes.
The insurance regulator can also oversee Ayushman Bharat. Currently, the healthcare programme is hobbled. There are not enough doctors. India has just 1.3 hospital beds and 0.8 physicians for every 1,000 people.
India is not testing enough, so the credibility of figures being shared by the ministry of health is being questioned. “Bihar has only one testing centre. . . Having just 52 centres across India makes no sense. And not even all of these are fully functional,” Dr T Sundararaman, a former director of the National Health Systems Resource Centre, has said. Bihar, one of the poorest states in India, has reported only four cases and one death, so far.
Again, insurance companies can league up with the likes of the UK-based Mologic Ltd, in collaboration with Senegalese research foundation Institut Pasteur de Dakar, which in three months promises to bring down the cost of COVID-19 testing kits to just $1 and testing time to10 minutes. That could be a game-changer.
For now, there is a lockdown for three weeks. Much of the business will be crippled but the government can use these 21 days to overhaul the medicare sector.
(Series concludes)(The author is a consulting editor with Moneycontrol)Discover the latest Business News, Sensex, and Nifty updates. Obtain Personal Finance insights, tax queries, and expert opinions on Moneycontrol or download the Moneycontrol App to stay updated!
Find the best of Al News in one place, specially curated for you every weekend.
Stay on top of the latest tech trends and biggest startup news.